

Chronic venous disease (CVD) is a chronic condition related to or caused by veins that become diseased or abnormal.
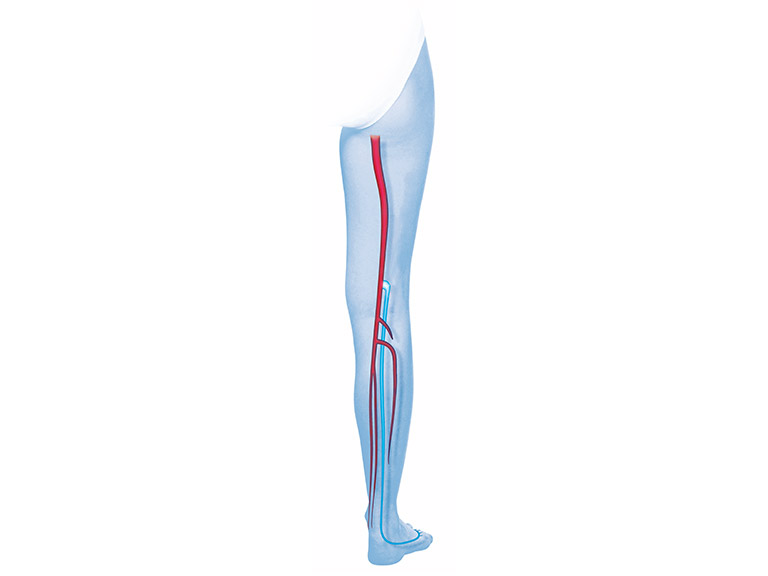
It is a very common disease with progressing severity. Early symptoms of chronic venous disease are a sensation of swelling and heaviness, most commonly in the legs. If the disease progresses varicose veins occur. Left untreated, varicose veins can enlarge and worsen. As a result, the symptoms will become more severe e.g. irritation, swelling and painful rashes.
Severe pooling of blood in the veins slows the return of blood to the heart. This can lead to condition can cause deep vein thrombosis and pulmonary embolism. Another potential consequence is chronic venous insufficiency (CVI), which leads to skin changes and development of venous leg ulcers (VLU).
VLUs have a big impact on the daily life, they can be painful, so that the ability to work may be compromised.
Without proper treatment, these potential consequences of chronic venous disease can lead to prolonged disability and have an important socioeconomic impact, and significant psychosocial morbidity.
Due to the potential seriousness of chronic venous disease, it is very important to be correctly diagnosed in good time. The problem will not go away, and the earlier it is diagnosed and treated, the better the chances of preventing serious complications.
There are several procedures that can be used alone or in combination to treat CVD.
In particular, compression therapy is considered the corner stone of treatment for chronic venous disease. Compression bandages and stockings gently compress the legs and help to improve blood flow in the veins by preventing backward flow of blood. Nevertheless, in some cases compression therapy cannot be applied and venous surgery may be necessary.